Experienced Specialists.
Compassionate Staff, State of the Art Treatments.



Our mission is to be a solutions based practice, maximizing the value of the service we deliver our patients with a commitment to excellence, integrity, innovation and treatment. We continually strive to provide comprehensive state of the art urological services with emphasis on patient education and shared decision making. Treating patients with compassion, dignity, mutual respect, and trust remains out steadfast goal. We will strive to be the urology group of choice in the communities we serve.
Innovation and industry-leading treatments, diagnostics, and surgical techniques are integral parts of our practice.

Rezūm Water Vapor Therapy treats the source of BPH — your enlarged prostate. This short, in-office procedure uses the natural energy stored in a few drops of water to shrink the prostate.

The Urolift system uses tiny implants to hold open the obstructed pathway that’s blocking urine flow, addressing the blockage, not just continuously treating enlarged prostate (BPH) symptoms. Most patients return home immediately and experience a speedy recovery.
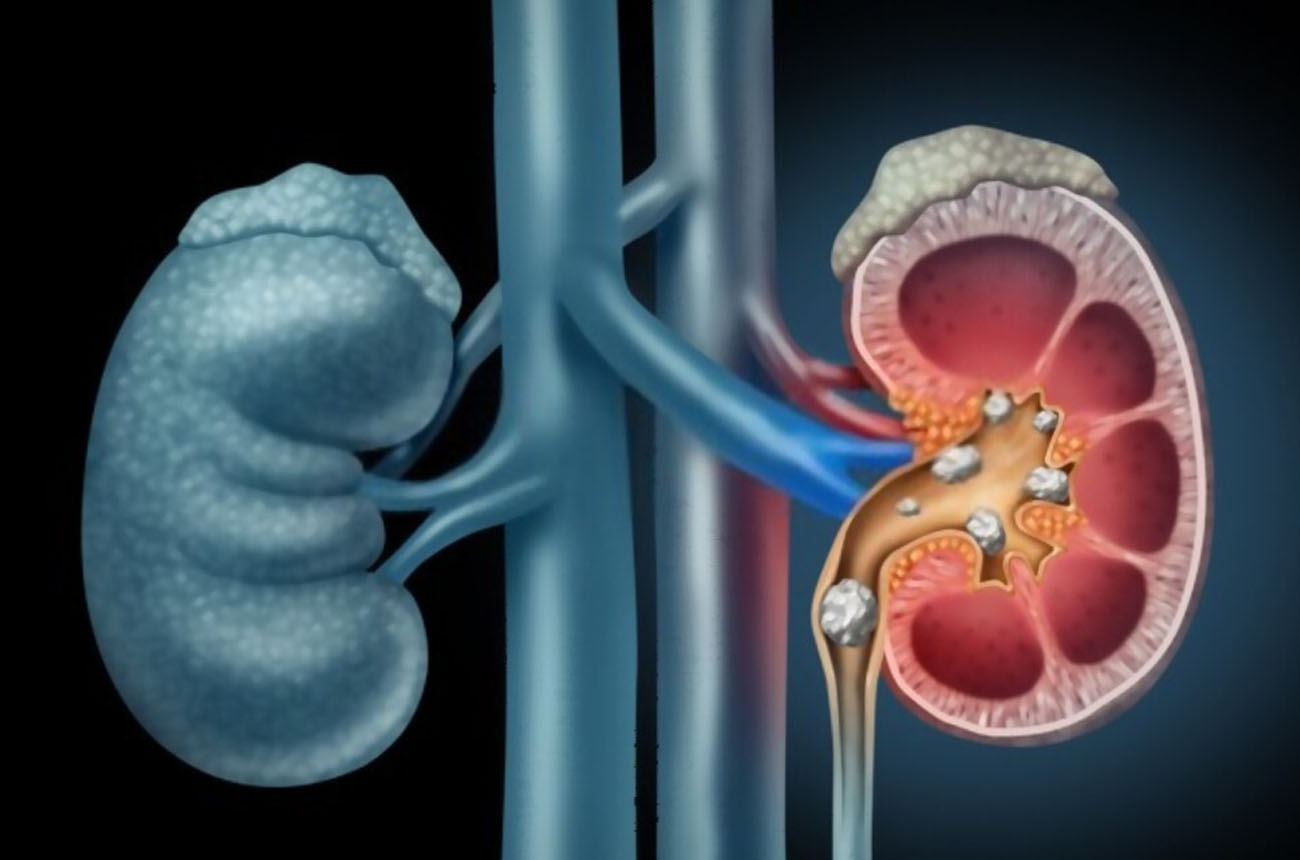
At UUANJ we use the latest technologies to treat Kidney, Ureteral, and Bladder stones. Our doctors are trained in the most advanced treatments including minimally invasive options for the treatment of stones.
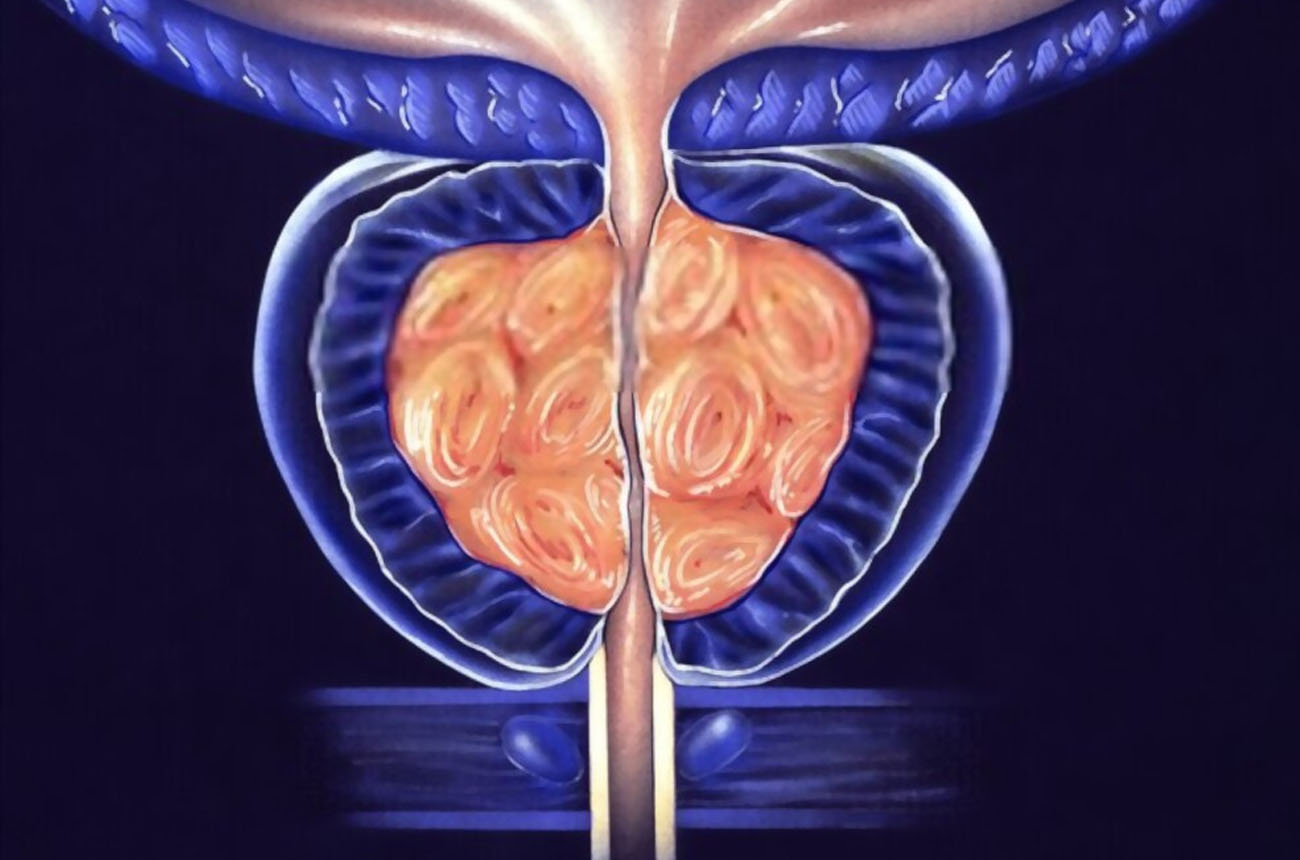
Plasma Vaporization & Resection of the prostate uses low-temperature energy to safely remove tissue. This technology allows for shorter procedure time, less bleeding, and quick recovery when compared to the traditional TURP procedure.

Our team of doctors has performed thousand's of vasectomies and experience matters. The UUANJ team has streamlined the vasectomy process. We offer vasectomies in-office and outpatient surgical centers.

SpaceOAR Hydrogel is an absorbable hydrogel that temporarily creates space between the prostate and the rectum, reducing the radiation dose delivered to the rectum during prostate radiation therapy.

UUANJ offers the latest treatment for overactive bladder including Surgical implantation of Neuro stimulator devices to help treat bladder dysfunction. We are an InterStim center of excellence.

BOTOX® is placed in the bladder muscle about every 6 months to target the source of your OAB. When you inject Botox for the bladder, the drug helps block certain nerves from communicating with the sphincter muscles or the bladder itself, relieving certain bladder symptoms such as the inability to delay urination.

UUANJ is proud to offer treatment of erectile dysfunction including medical and surgical treatments.

We are pleased to offer Robotic and Minimally Invasive Surgery to our patients. Our robotics team is trained in the latest advancements in these procedures.
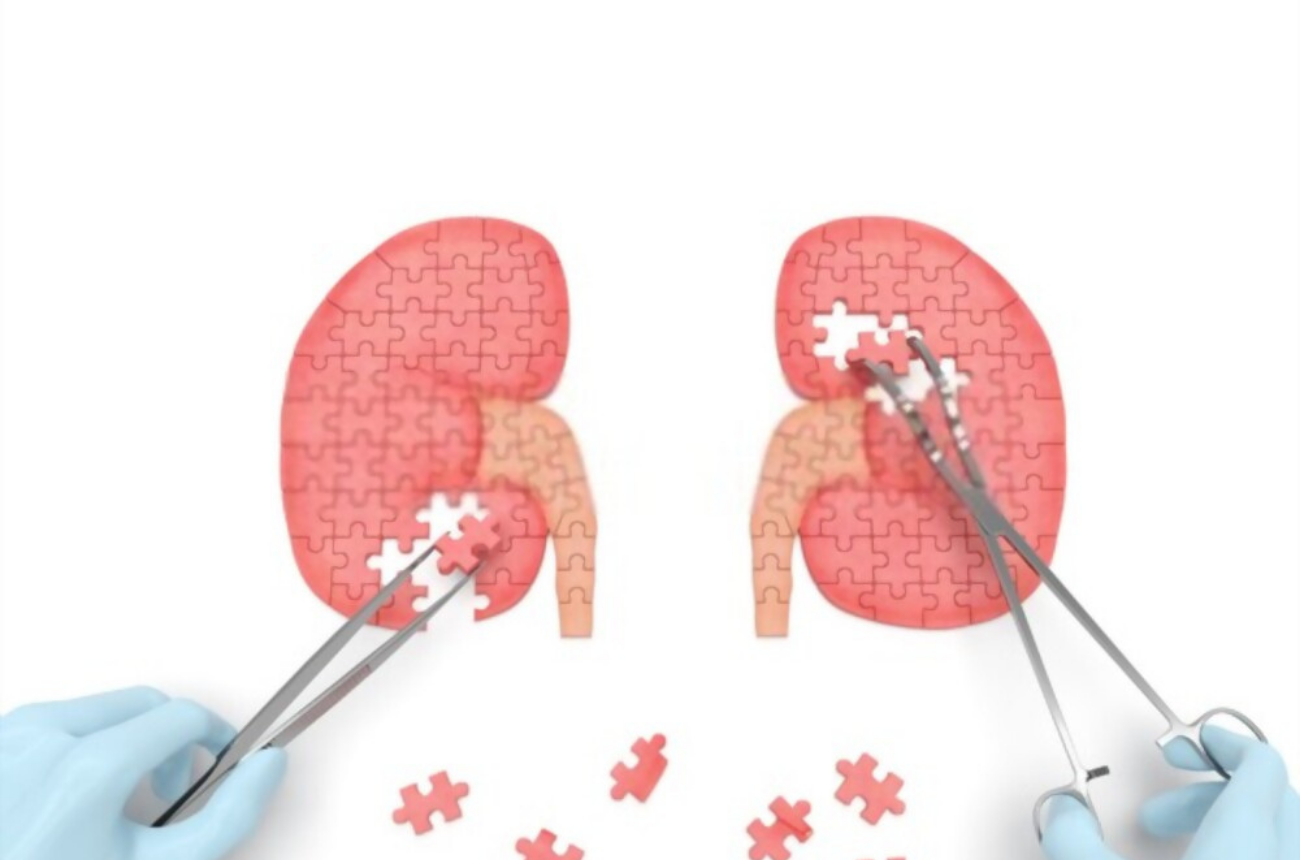
Our UroOncology team at UUANJ has performed many partial and radical nephrectomies using minimally invasive and open techniques.
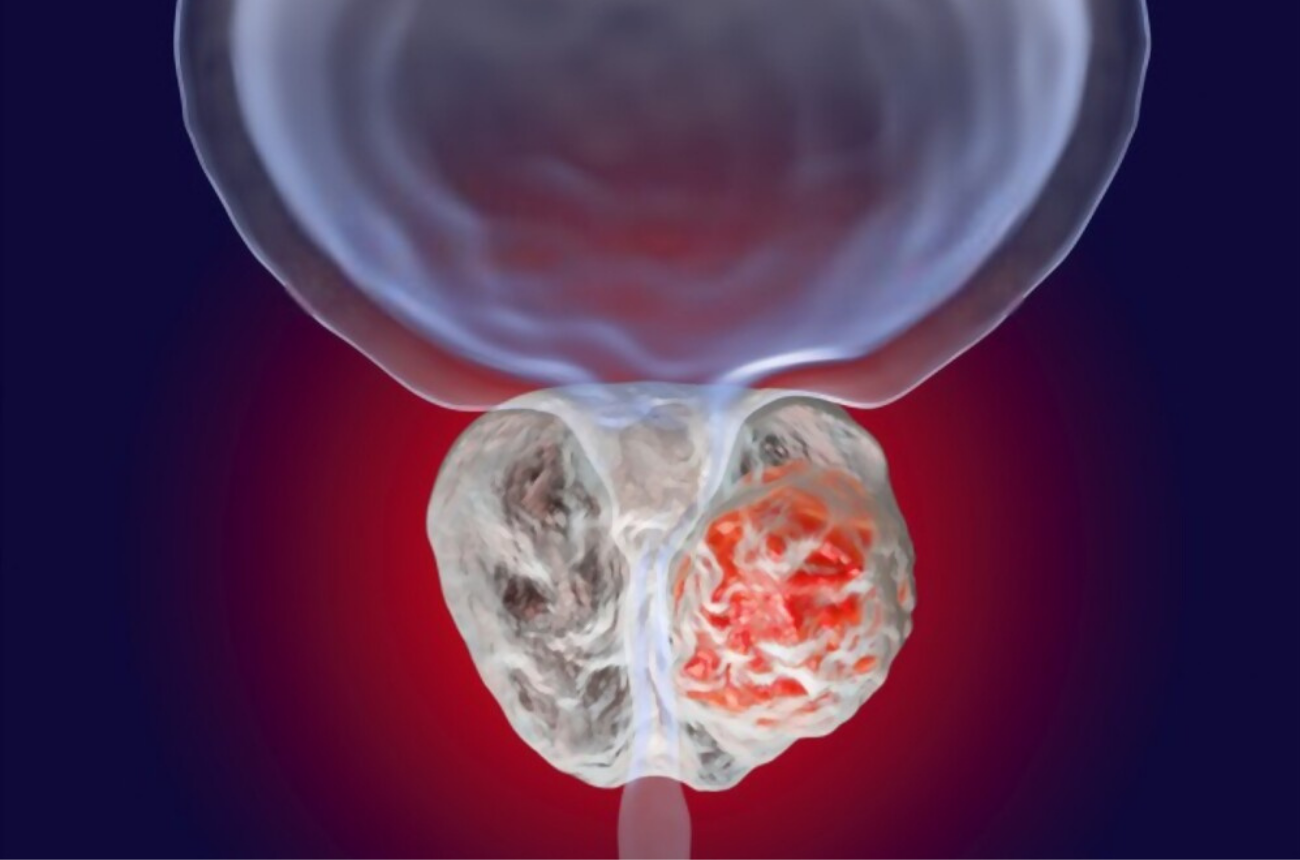
We are able to offer prostatectomy surgery to qualified patients for both cancer and non-cancerous treatment options. This includes the Robotically Assisted Laparoscopic Prostatectopy (RALP)

Our Urology team at UUANJ in New Jersey specializes in diagnosing and treating conditions of the male and female urinary tract, and male reproductive system. The team believes in treating you with comprehensive and compassionate care ― not simply treating your diagnosis or condition. We're available to provide a first or second opinion for simple to complex conditions affecting your urinary tract or reproductive system.

Our team is guided by world-class doctors having these values: The needs of our patient come first. We place your needs above all else.

Our team treats common or complex urologic conditions using the latest therapeutic procedures, diagnostic equipment and minimally invasive techniques.

Our urology team works collectively to develop a treatment plan for each patient. We collaborate with Internal Medicine, OB-GYN, Pediatrics and Oncology to ensure you are receiving the care you need.

Our primary goal will always be focused on developing the right treatment plan to meet your individual needs. Our team offers in-person and virtual consults to deliver care where convenient for you.



Check out UUANJ's blog that keeps you updated on education you need to know to stay healthy and keep informed about your urological health.


